
By STEPHEN BORSTELMANN, MD
Occasionally, you get handed a question you know little about, but it’s clear you need to know more. Like most of us these days, I was chatting with my colleagues about the novel coronavirus. It goes by several names: SARS-CoV-2, 2019-nCoV or COVID-19 but I’ll just call it COVID. Declared a pandemic on March 12, 2020 by the World Health Organization (WHO), COVID is diagnosed by laboratory test – PCR. The early PCR test used in Wuhan was apparently low sensitivity (30-60%), lengthy to run (days), and in short supply. As CT scanning was relatively available, it became an important diagnostic tool for suspected COVID cases in Wuhan.
The prospect of scanning thousands of contagious patients was daunting, with many radiologists arguing back and forth about its appropriateness. As the pandemic has evolved, we now have better and faster PCR tests and most radiologists do not believe that CT scanning has a role for diagnosis of COVID, but rather should be reserved for its complications. Part of the reason is the concern of transmission of COVID to other patients or healthcare workers via the radiology department.
But then someone asked: “After you have scanned a patient for COVID, how long will the room be down?” And nobody really could answer – I certainly couldn’t. A recent white paper put forth by radiology leaders suggested anywhere from 30 minutes to three hours. A general review of infection control information for the radiologist and radiologic technologist can be found in Radiographics.
So, let’s go down the rabbit hole of infection control in the radiology department. While I’m a radiologist, and will speak about radiology-specific concerns, the fundamental rationale behind it is applicable to other ancillary treatment rooms in the hospital or outpatient arena, provided the appropriate specifics about THAT environment is obtained from references held by the CDC.
The basics that you know:
Patients transported to the radiology department should be covered by a clean sheet and wear a mask. HCPs with direct patient contact with suspected or confirmed COVID patients should use their personal protective equipment (PPE), including a N95 or P99 mask or respirator, eye coverage, gloves, and gown.
What you might not know:
Currently, COVID is thought to be spread by respiratory droplets or direct contact with contaminated surfaces. It is not believed to transmit by a frank airborne route. However, a small infection control study during an outbreak of the MERS coronavirus was concerning for either fomite vectors or a transmission mechanism in between droplet and airborne, with the smallest droplets instantly desiccating in air, resulting in transmission beyond 6 feet. CDC recommendations published in 2003 include a delay in terminal cleaning until air exchange has removed potentially infectious particles. In radiology diagnostic suites, with a minimum recommended 6 total air exchanges per hour (ACH), 99% efficiency in particle removal is 46 minutes and 99.9% removal is 69 minutes. For radiology angiography suites, with a higher recommended minimum ACH/hr of 15, 99% efficiency in particle removal is 18 minutes and 99.9% removal is 28 minutes. The formulas for calculating the ACH and the time until reaching particulate clearance are given below:
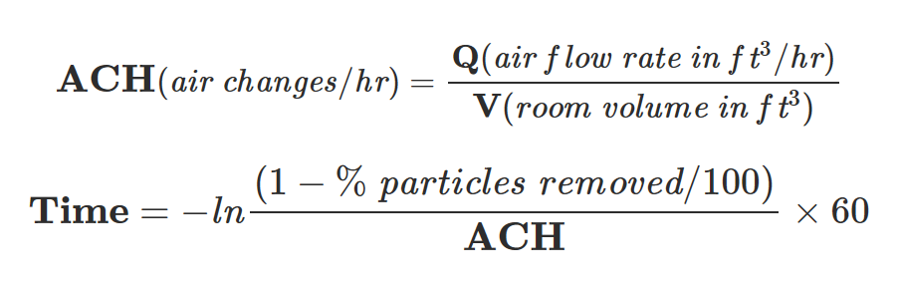
% of particles removed is 99 or 99.9 as given above

Of course, there are assumptions in these calculations, and if your facility is actively treating COVID patients, you may want to meet with your facilities management team for a more definitive answer.
One major assumption is that there is not sustained virus released – something that might not be true in a ventilated patient. In fact, activities that create aerosols, like mechanical ventilation, CPAP/BiPAP, suctioning or intubation can cause COVID to remain aerosolized for up to three hours.
Surface Cleaning:
After waiting a safe period for air exchange, terminal cleaning should be performed. COVID has been shown to survive up to 72 hours on plastic and stainless steel, and about a day on cardboard. All Radiology and CT equipment are classified by OSHA and the CDC as non-critical surfaces for disinfecting, contacting intact skin only (in the absence of open wounds, surgery or trauma). This includes the gantry, padding, bore, cassette, and portable x-ray machines. Long-handled sponges have been used to clean CT/MRI bores.
Right now there is no cleaning agent of choice for COVID. Surfaces can be decontaminated by intermediate level disinfectants (bleach, isopropyl alcohol, various commercial preparations) or low-level disinfectants (any intermediate solution used < 10 minutes; ammonium solution). Intermediate level disinfectants typically kill more viruses than low-level disinfectants. You’re probably already using one right now! Ask facilities engineering or housekeeping for your institutions preferred cleaner.
Common sense would suggest that all non-critical equipment, including cleaning supplies, are put away in cabinetry or outside of the room and no open boxes, etc., are on countertops or floors. Previous recommendations made during SARS were to pay attention to cleaning frequently touched surfaces, remove unnecessary supplies and equipment to facilitate frequent cleaning, and avoid carpets if possible, vacuuming daily while in PPE if not.
Discussion:
A fear in pandemics is the overwhelming of hospital system capacity by the infected. As a single confirmed COVID patient can take down a CT or MR suite for anywhere between 1 and 3 hours, depending on whether they are ventilated, this is a reasonable concern. The rate-limiting step in minimizing downtime and enhancing throughput will be air exchange. The following common-sense suggestions may be helpful:
First and foremost, PCR is the test of choice for COVID diagnosis. ‘R/O COVID’ using CT is not encouraged.
Second, a lot of information can be obtained by a portable chest x-ray. Portable chests need not worry about room gas exchange and can increase diagnostic confidence. They can even be performed through glass!
Third, for facilities that have multiple CT scanning suites, consider reserving one for confirmed positive COVID cases and another for non-COVID patients presenting for other reasons (trauma, RLQ pain, stroke). Institutions with multiple scanners can allocate dynamically to COVID positive vs. negative patients based upon daily census and incidence.
Fourth, increasing throughput in the scanners dedicated to COVID patients is challenging particularly when ventilated patients are scanned. Scanning ventilated COVID patients in the same scanner back-to-back may not increase risk to patients, but instead expose HCP’s to sustained droplet aerosols with high viral titers, increasing the risk of HCP infection. Fitted full-face respirators should be given to these HCPs. Room air flow can be increased to clear particles more quickly by portable Negative Pressure Devices (NPDs) – essentially portable blowers – which increase room air flow (Q), and thus ACH. Such devices need to be used properly, and optimally are vented outside the building to an area 25 feet away from public access or air intakes.18 Facilities engineering needs to be involved in their use. It is conceivable that by using one of these devices with proper exhaust and a dedicated cleaner on-site with a one-minute certified cleaning agent, three scans an hour could be attempted – see figure 3
Figure 3 – CT patients and estimated TATs
(estimated only)
| Patient | Scan Time | Air Exchange Time | Cleaning Time | Total Turnaround Time (TAT) |
| Non-COVID ‘r/o bleed’ | 5 minutes | N/A | 10 minutes | 15 minutes |
| Suspected COVID CT chest | 5 minutes | 46 minutes | 10 minutes | 61 minutes |
| COVID + on Ventilator | 5 minutes | 180 minutes | 10 minutes | 195 minutes |
| COVID + CT Chest with NPD* | 5 minutes | 15 minutes | 10 minutes | 30 minutes |
| COVID + CT Chest with NPD* and 1min cleaning solution | 5 minutes | 15 minutes | 1 minute | 21 minutes |
*NPD = negative pressure device
Fifth, much elective or non-urgent follow-up care has been temporarily curtailed to create reserve capacity if a potential surge in infections manifests. However, eventually those patients will need their follow-up care. It may be preferential to shift routine imaging to outpatient facility scanners except for chest and thorax imaging, which can be scheduled in the hospital – in order to avoid the inadvertent identification of pulmonary ground-glass opacities at the outpatient facility. That would likely prompt an hour-plus long shutdown and cleaning & perhaps the closure of the facility for the day. Alternatively, in the hospital, the patient then can be guided for PCR testing (if appropriate) and cleaning can be done by an experienced staff with full PPE who will be less likely to self-infect.
The number of outpatient imaging studies performed needs to be carefully coordinated with local hospital capacity, as an unexpected finding may then prompt hospital presentation, theoretically increasing the patient’s risk of infection and further straining limited hospital resources. A flowchart illustrating one possible decision rationale is shown in Figure 4:

As we are in the early days of the COVID pandemic, the preceding is only a list of suggestions based upon the best available data at this time. These should be tailored to the specific needs of the individual radiologist and their facility. While CT scan and portable chest x-ray were examples, these recommendations would generally apply to ANY diagnostic imaging modality or treatment room involved in the care of COVID patients. As other patient care areas are designed with different baseline air flow rates, the CDC’s guidelines for environmental infection control, including Appendix B can be helpful for those specific areas.
Stephen M Borstelmann MD is an interventional radiologist and published medical AI researcher/speaker with an interest in operations.
The post Infection Control for COVID-19 Imaging appeared first on The Health Care Blog.
